Perfect B, Doral Fl. | 12.11.25 | 5 min read.
Perimenopause can feel confusing enough on its own. Add the desire for a baby in your forties or early fifties and it is no surprise that searches like “perimenopause or pregnancy” and “can you get pregnant during perimenopause” are so common. This article walks you through what is happening with your hormones, how fertility really changes, and where regenerative approaches may or may not fit into a safe late age pregnancy plan, all from a regenerative medical perspective that considers tissue health and long term wellbeing.
What Is Perimenopause and Why Are Periods So Irregular?
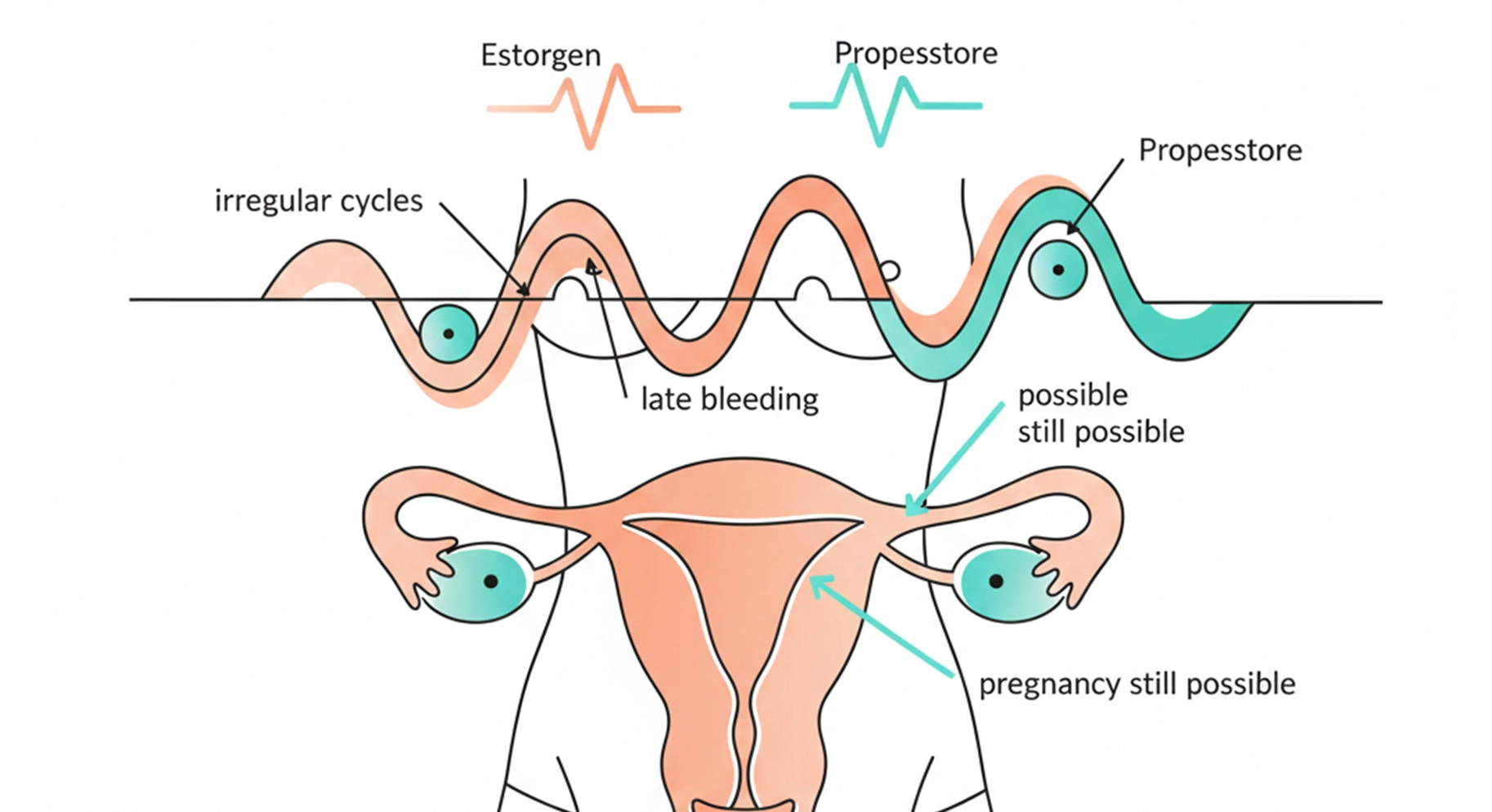
Perimenopause is often described as a second puberty in women. Your ovaries still work, but estrogen and progesterone fluctuate instead of following a predictable monthly pattern. That hormonal roller coaster explains why many people notice irregular periods and perimenopause happening at the same time. For many patients, irregular periods and perimenopause arrive together with changes in sleep, mood and energy. Some cycles are shorter, some are longer, and some months there is no bleeding at all.
From a patient point of view, this might look like perimenopause and irregular periods or irregular cycles perimenopause where you can no longer set your calendar by your period, and it may feel as if irregular periods and perimenopause have taken over your planning. Clinically this is a form of irregular menstruation menopause transition, not yet full menopause. You may also see symptoms such as night sweats before period, breast tenderness or mood swings even when the bleed itself is lighter or later than usual.
As ovulation becomes erratic, some cycles include an egg release and others do not. That is why a person can ask, “why am I not ovulating but having periods” or wonder whether a period without ovulation signs really counts. Bleeding alone does not guarantee that ovulation happened. It simply means the uterine lining is shedding.
Over time you may notice signs of end of perimenopause, such as longer gaps between cycles, or signs perimenopause is ending, such as going many months without bleeding. At that point, even one period during perimenopause can raise questions about what is normal.
Some people panic if they are 2 weeks late menstruation, others worry about a period late perimenopause that shows up after they thought everything had stopped, and many are simply unsure if what they are feeling is perimenopause or pregnancy. All of these patterns can be part of the transition, but big shifts, especially with pain or heavy flow, deserve a check in with your clinician.
When clinicians explain potential detriment define, they often mean the ways that unmanaged symptoms or missed diagnoses can harm long term health. Understanding the pattern of your cycles helps your team distinguish normal transition from problems that need treatment.
Late or Heavy Bleeding Versus Pregnancy: What Is Normal and What Is Not?
Because cycles become unpredictable, it is easy to confuse perimenopause changes with early pregnancy and to feel uncertain about whether symptoms reflect perimenopause or pregnancy. When irregular periods and perimenopause overlap with heavy flow, clots or pain, it becomes even more important to check in with a clinician. Someone who is menstruation late for 2 days may be dealing with hormones, stress or a conception. A delay of two weeks or more, especially if you are sexually active, should trigger a pregnancy test and a conversation with your provider.
Heavy or prolonged bleeding should never be ignored. Heavy bleeding perimenopause and heavy periods in perimenopause can be related to hormone changes, but they can also signal fibroids, polyps, clotting problems or in rare cases cancer. If you are soaking through products quickly, passing clots or experiencing perimenopause bleeding for 3 weeks, seek medical care promptly.
Spotting patterns matter as well. Light spotting in perimenopause can happen when hormone levels dip, but perimenopause and spotting between periods, perimenopause spotting between periods or bleeding after sex can point to infections or structural changes. Add strong cramps no period perimenopause and it is even more important to rule out pregnancy or other pelvic problems.
Clinicians worry about detriment when heavy or irregular bleeding leads to anemia, fatigue or missed diagnoses. The goal of evaluation is not to pathologize every change, but to be sure that concerning patterns are not overlooked.
The bottom line is that irregular bleeding is common, but persistent, painful or very heavy changes should never be written off as just hormones.
Can You Get Pregnant During Perimenopause If Your Cycles Are Irregular?
Short answer, yes. As long as ovulation occasionally occurs, pregnancy remains possible. Your ovaries may still release eggs even if it does not happen every cycle. That is why so many people search can you get pregnant during perimenopause, premenopausal can you get pregnant or can premenopausal woman get pregnant. When you wonder can you get pregnant during perimenopause and see conflicting information online, it is natural to feel unsure about your next steps.
From a clinical standpoint, perimenopause pregnant and pregnant in perimenopause are both real world scenarios. The challenge is that ovulation becomes less predictable, so the window for conception is harder to track. People who assume they are too old to conceive may be surprised by a positive test, while others who are actively trying may struggle.
When patients ask can you get pregnant on perimenopause or can perimenopause woman get pregnant, we explain that fertility does decline, but it rarely drops straight from normal to zero. Even with irregular periods and menopause approaching, isolated ovulations can still occur, so irregular periods and perimenopause do not mean that pregnancy is impossible. That is why contraception is recommended until you have had 12 months with no bleeding at all.
If your goal is a baby, your team will look at age, ovarian reserve and overall health, then discuss realistic options. If you absolutely do not want to be pregnant, irregular cycles are not a reliable form of birth control, and a surprise conception can sometimes carry higher medical risk than a planned pregnancy matched to your health status.
What Is Regenerative Medicine in Women’s Health?
Patients often hear about regen med, regen therapy or regeneration therapy and wonder if these approaches could bypass age related limits on fertility. Before answering that, it helps to look again at detriment define, the potential harm of overselling unproven treatments while downplaying their risks.
In simple language, the meaning of regenerative is the ability to repair or rebuild tissue instead of just masking symptoms. Regenerative medical approaches may use living cells, growth factors, biomaterials or devices to stimulate healing. In women’s health, research is exploring endometrial stem cells for uterine scarring, biologic meshes for pelvic floor support and techniques to improve blood flow and tissue quality. For our clinic, regenerative medical thinking means asking how these discoveries might eventually support safer, evidence based care rather than promising quick fixes.
Working in regenerative medicine naturally brings questions that touch many areas of a patient life. For women who are wondering can you get pregnant during perimenopause or who are already close to menopause, there is understandable interest in future regenerative options that may one day target ovarian reserve or egg health directly. At this time those therapies are still in development, but our role at Perfect B is to focus on the evidence based ways we can support you right now while you work with a fertility specialist on the reproductive side.
When people hear rejuvenation define or see spa advertisements for ovarian rejuvenation, they sometimes imagine egg cells being turned back in time. In reality, most true regenerative techniques that affect fertility are still in the research stage. They are not yet standard choices alongside options such as in vitro fertilization or donor eggs.
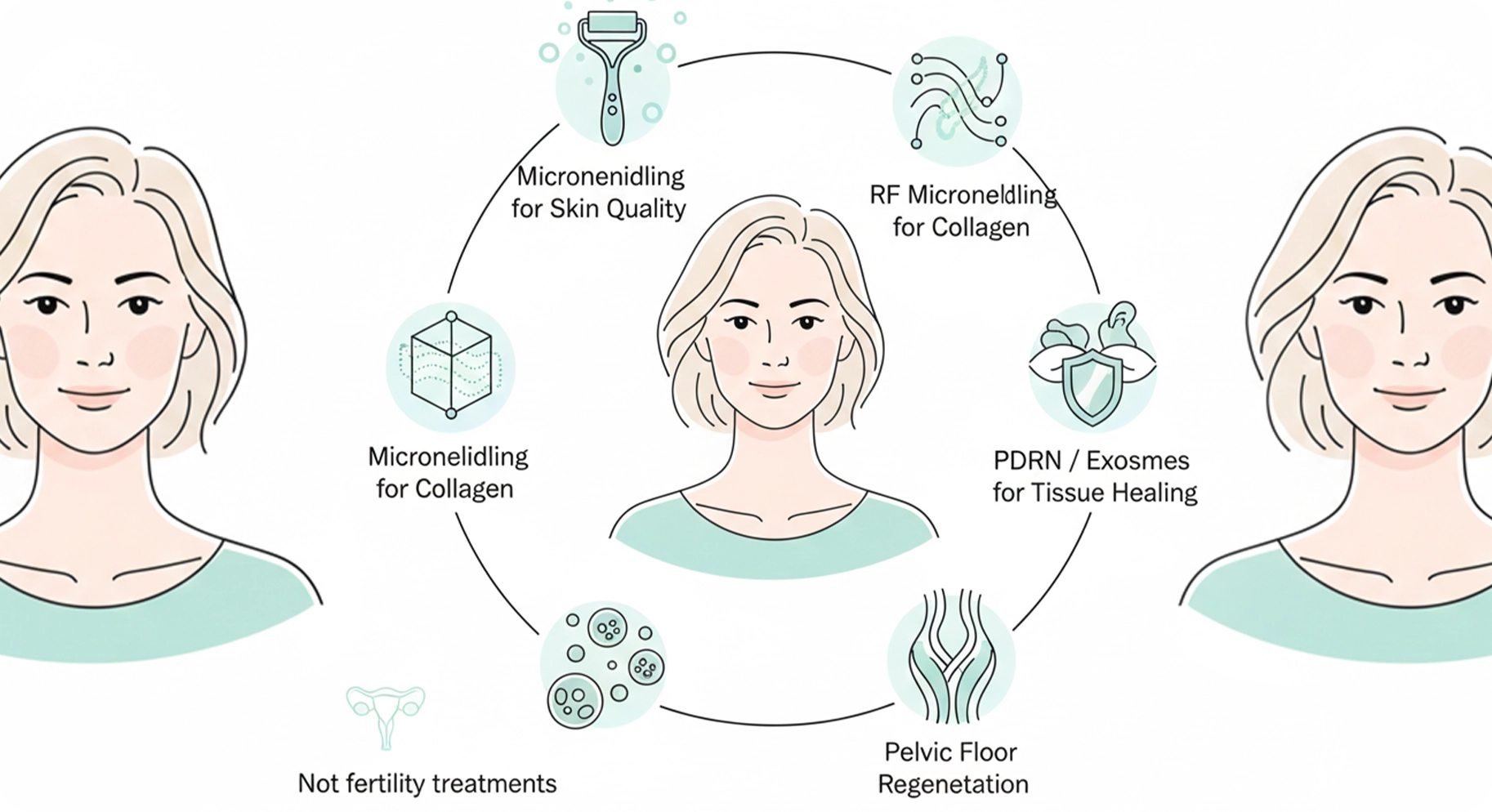
Where does aesthetic medicine fit in this picture. Local procedures that focus on skin regeneration, for example microneedling or laser resurfacing, aim to answer the everyday question does skin regrow in a healthier way after controlled injury. For the most part, these treatments target the skin only, not the ovaries or uterus, and they are not fertility treatments.
Popular Regenerative and Anti Aging Therapies: What We Know About Fertility and Pregnancy Safety
Marketing language moves faster than evidence. Many people who are considering late age pregnancy also read about peptides therapy, exosomes, stem cells or various supplements and ask if these options will make conception easier or safer.
Here at Perfect B we position these tools as supplemental support rather than fertility treatments. NAD protocols are used to support cellular processes that decline with age, while exosomes, PDRN and PRP are directed toward improving skin quality and texture through a series of carefully planned treatments that often combine microneedling or RF microneedling to enhance absorption. These regenerative strategies can help you feel more at ease in your changing body, but they are not a substitute for a full fertility workup.
Some clinics promote injections that use mesenchymal cells or tissue based products as part of regenerative medical packages. Search terms such as stem cell injections cost reflect how attractive these offerings can seem. At the same time, most stem cell based fertility interventions remain experimental, and the long term safety, especially in someone who is pregnant or trying to conceive, is not well established. The same caution applies to exosome treatment, which involves packages of signaling molecules released by cells, interesting in the lab but far from a guaranteed fertility solution.
You may also see neuropathy supplements or nerve support products advertised online, including brands such as Nerve Renew. These may have uses for nerve pain, but they have not been proven as tools to restore ovarian reserve or make late age pregnancy safer.
NAD related therapies are another frequent topic. People search phrases like nad benefits for women 1 or nad for women hoping for a simple solution. Many popular articles about nad for women focus on energy, focus and anti aging, not on careful pregnancy safety data. Nicotinamide adenine dinucleotide, usually shortened to NAD, is a molecule involved in cellular energy and repair, and some early research suggests potential benefits in aging biology, but there is limited human data in pregnancy.
Questions such as can you take nad while pregnant, can I take nad while pregnant, is nad safe during pregnancy, nad and pregnancy, nad pregnancy, nad supplement pregnancy or nad supplement for fertility all point to the same reality. Evidence on nad for women in pregnancy is still sparse, and decisions should be made with your obstetric or fertility specialist. At this time we do not have robust safety data.
For now, any NAD boosting protocol, whether infusions, high dose oral products or combinations with other agents, should be considered experimental in someone who is pregnant or actively trying to conceive. From a safety point of view, nad for women who are not pregnant is a very different conversation from nad for women who are already pregnant or trying to conceive.
➔ If you mainly want to understand how we use NAD and other regenerative tools in non pregnancy protocols for energy, recovery and skin regeneration, you can read more on our Regenerative Medicine Treatment page where we describe our consultation flow and follow up schedule and explain how we think about nad for women in general anti aging programs. This does not automatically mean NAD is harmful, but it does mean that you and your obstetric or fertility specialist should discuss potential risks and benefits before starting or continuing such treatments.
In our practice we may use carefully selected regenerative tools to support recovery, tissue health and skin regeneration, but we do not present them as shortcuts to late age pregnancy or as substitutes for evidence based fertility care. Our regenerative medical team focuses on realistic goals that fit within your broader medical plan.
How to Safely Plan Pregnancy in Perimenopause
If you are contemplating a baby while your cycle is changing and you keep asking yourself can you get pregnant during perimenopause, you do not need to navigate it alone.
Start with a full medical and fertility evaluation.
A reproductive endocrinologist or obstetric clinician can assess ovarian reserve, overall medical risk and how your irregular periods and perimenopause changes affect timing and treatment choices. They will also review medications, supplements and any regenerative procedures you are considering.
Clarify your priorities and timeline
Because egg quantity and quality decline with age, waiting several years may significantly reduce the chance of pregnancy, especially if you already wonder how long you can get pregnant during perimenopause before fertility drops further. A specialist can explain options ranging from timed intercourse to in vitro fertilization or donor eggs for someone who is perimenopause pregnant or hoping to be.
Coordinate all treatments.
If you are using any regenerative or anti aging approaches, NAD products, regen therapy, aesthetic procedures or complementary care, share that list with your fertility and obstetric team.
Use support services.
Emotional stress is a real detriment to quality of life during this process, even if it does not directly change fertility. Counseling, group support and mind body techniques can help you cope with uncertainty while medical decisions are made.
Apart from regenerative support and daily health habits such as nutrition, movement and appropriate supplements, the most important medical step if you are trying to conceive is to see a fertility specialist. Infertility can present differently in each person and can have multiple causes. A fertility workup looks at both you and your partner to understand what is happening in your specific case. At Perfect B our regenerative and skin focused treatments are designed to help you feel and function at your best, to reduce stress and support confidence, while your fertility team focuses on ovulation, egg quality and pregnancy safety.
Frequently Asked Questions
Q1: Can a perimenopausal woman get pregnant naturally
Yes. As long as ovulation sometimes occurs, pregnancy remains possible. This is why people ask can perimenopause woman get pregnant and similar questions. The chance of conception per month is lower than in the twenties or early thirties, and miscarriage risk is higher, but pregnancy is still possible until twelve consecutive months with no bleeding have passed.
Q2: How do I know if my symptoms are perimenopause or pregnancy
Symptoms overlap. Fatigue, breast tenderness, mood swings and nausea can appear in both perimenopause or pregnancy, which is why so many people search can you get pregnant during perimenopause when new symptoms appear. A home test and a clinic visit are more reliable than guessing. If you have irregular periods and menopause approaching and suddenly feel different, it is safer to check rather than assume.
Q3: When should I worry about late or missed periods
A period late perimenopause is common, but if you are sexually active and more than two weeks late, or menstruation late for 2 days plus new symptoms such as nausea or breast tenderness, especially on top of a history of irregular periods and perimenopause, testing is reasonable. Persistent late cycles, especially with pain or heavy bleeding, always deserve evaluation.
Q4: What about spotting or cramps between periods
Light spotting in perimenopause may be hormonal. However, perimenopause and spotting between periods, perimenopause spotting between periods, repeated spotting perimenopause or strong cramps no period perimenopause should prompt a visit. It is important to rule out infection, polyps, pregnancy complications or precancerous changes.
Q5: Do regenerative or anti aging therapies replace fertility treatment
No. Techniques such as regeneration therapy, regen med protocols, peptides therapy, exosome treatment or NAD based approaches may support recovery, comfort or appearance, but they are not proven replacements for conventional fertility care. Questions about whether does skin regrow more youthfully after these treatments are different from questions about restoring egg reserve or guaranteeing a healthy pregnancy.
If you are considering any of these options while trying to conceive or while pregnant, discuss them in detail with your fertility specialist and obstetric team before proceeding.
Disclosures, Partner Organisations and References
Our clinic collaborates closely with board certified obstetric and reproductive endocrinology specialists. We do not offer experimental stem cell based fertility procedures or unproven ovarian rejuvenation programs, and we do not claim that NAD products or exosome based therapies or any protocol marketed as nad for women can guarantee pregnancy at any age.
Key partner organisations
- Fertility Center Name, reproductive endocrinology and in vitro fertilization services.
- Hospital or academic partner, high risk obstetric and research support.
Selected references, DOIs to be added by the editorial team
- Educational reviews on nad for women in the context of healthy aging and metabolic support.
- Clinical guidelines on perimenopause and menopause management.
- Reviews on regenerative approaches in women’s pelvic and reproductive health.
- Articles evaluating NAD biology and aging in human health.
If you are navigating perimenopause and thinking about pregnancy, or already pregnant in perimenopause, the most important step is a personalised plan that is built with trusted clinicians who understand both the opportunities and the limits of regenerative medicine today.
➔ Book your Consultation. Get availability through Contact and Booking.



